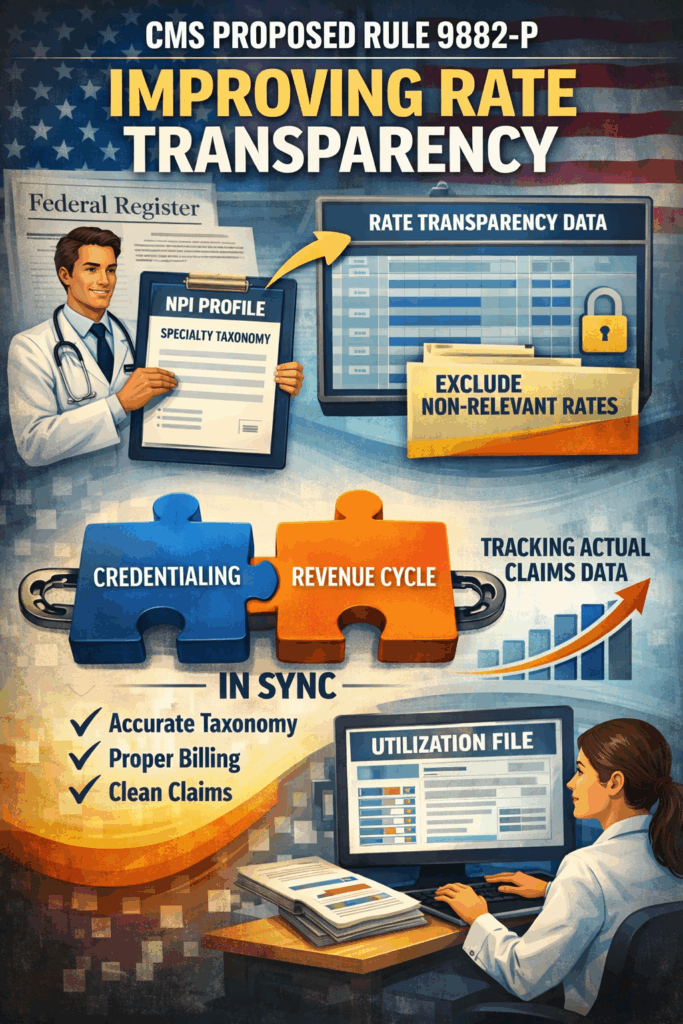
The proposed rule can be accessed via the Federal Register.
These proposed changes build on the historic disclosure requirements the Departments issued in the Transparency in Coverage final rules on November 12, 2020 (the 2020 final rules) in line with the President’s June 24, 2019, Executive Order (EO) 13877, “Improving Price and Quality Transparency in American Healthcare to Put Patients First.”
The primary cause of large In-network Rate File sizes is the inclusion of providers associated with negotiated rates for items or services they would be unlikely to furnish (e.g., rates for podiatrists to perform heart surgery). This occurs because payer-provider contracts often account for all items and services for all their providers, irrespective of clinical specialty.
To address these unlikely provider-rate combinations, the proposed rules include proposals to:
1) require group health plans and health insurance issuers to exclude from their In-network Rate Files provider-rate combinations for items and services for providers that would be unlikely to be reimbursed for the item or service given that provider’s area of specialty. The proposal would require plans and issuers to determine which providers to exclude by using their internal provider taxonomy mappings used in the claims adjudication process;
2) require payers to post the internal provider taxonomy mapping they used to prepare the In-network Rate File; and
3) require plans and issuers to post a new file called a Utilization File for each In-network Rate File which would include all providers who have submitted and received reimbursement for at least one claim for a covered item or service over the 12-month period ending 6 months before the posting of the file.
RCM + Credentialing: The Hidden Link Under CMS Proposed Rule 9882-P
Over the years, every time I’ve onboarded a new physician or APP, I’ve noticed something interesting – their NPI profiles often still show taxonomy codes from residency days.
Whether it’s been 2 or 12 years since they graduated, those NPPES profiles are rarely updated.
I used to wonder: if taxonomy didn’t really affect payer credentialing and enrollment, why does NPPES even ask for it?
Well… it’s about to matter – a lot.
Under CMS Proposed Rule 9882-P, payers will be required to map their rate transparency data directly to provider taxonomy codes. On the surface, it’s a data organization requirement meant to make massive files more machine-readable.
But here’s the hidden impact:
Credentialing teams will now have to ensure every provider’s taxonomy is accurate and current.
At Cred2Bill, we’ve always encouraged tight collaboration between Credentialing and Revenue Cycle (RCM) teams. It’s the only way to ensure that:
- Providers are credentialed under the right specialty/sub-specialty;
- Billing setups mirror payer enrollments; and
- Claims flow and payments stay accurate and timely.
With CMS 9882-P, that interdependence is no longer optional – it’s essential.
Specialty (sub-specialty) = Accurate and Specific Taxonomy
In short, the days of overlooking NPPES taxonomy codes are over. Credentialing and RCM must move in sync not just to stay compliant, but to stay efficient.
#Credentialing #RCM #CMS9882P #HealthcareOperations #ProviderEnrollment